Pharmacy First Service
Pharmacy First , which includes providing advice and NHS-funded treatment, where appropriate, for seven common conditions will be launched on 31st January 2024 (subject to the required IT systems being in place) as an Advanced Service.
You can view the Pharmacy First Training Summary for a comprehensive list of Pharmacy First related training opportunities.
Further information is available on Community Pharmacy England
Consultations can be provided to patients presenting to the pharmacy as well as those referred by NHS 111, GPs and others. The service will also incorporate the existing Community Pharmacist Consultation Service.
In the consultations with a pharmacist, people with symptoms suggestive of the seven conditions will be provided with advice and will be supplied, where clinically necessary, with a prescription-only treatment under a Patient Group Direction (PGD).
Latest news on the service
Pharmacy First drop in sessions.
Community Pharmacy England held a series of online drop-in sessions around the launch date of the Pharmacy First service to answer any queries on the service.
On Demand Webinars
The webinars were hosted by Community Pharmacy England – available to view here on demand
Further details can be found on their news story. https://cpe.org.uk/our-news/implementing-pharmacy-first-drop-in-sessions-and-additional-resources
New resources
The pharmacist and pharmacy owner checklists (previously these were to “get going” with implementation of the service but they have been updated now that more resources have been published. Also a template letter/email template has been published that pharmacy owners can send to GP practices to make them aware of the new service. Links to these resources can be found in the news story. https://cpe.org.uk/our-news/implementing-pharmacy-first-drop-in-sessions-and-additional-resources
The Comms Team at CPE has also published a series of resources to help promote the new service to patients and members of the public including a selection of posters, suggested social media posts, etc media tiles. They are also working on content for digital screens so hopefully that will be available shortly. More information in the news story https://cpe.org.uk/our-news/pharmacy-first-resources-to-promote-the-service/
What does the service involve?
The new Advanced service involves pharmacists providing advice and NHS-funded treatment, where clinically appropriate, for seven common conditions; under a patient group directive (PGD)
- sinusitis
- sore throat
- acute otitis media
- infected insect bite
- impetigo
- shingles
- uncomplicated urinary tract infections in women.
Consultations can be provided to patients presenting to the pharmacy as well as those referred by NHS 111, general practices and others.
The service will also incorporate the existing elements of the Community Pharmacist Consultation Service, i.e. minor illness consultations with a pharmacist and the supply of urgent medicines (and appliances), both following a referral from NHS 111, general practices and other authorised healthcare providers.
Consultation fees and monthly fixed payment
Pharmacies will be paid £15 per completed consultation.
From February 2024, in addition to the £15 consultation fee, a monthly fixed payment of £1,000 will be paid to pharmacy owners who meet a minimum activity threshold of clinical pathways consultations (the threshold will increase over time as set out below).
| Month | Minimum number of clinical pathways consultations |
| February 2024 | 1 |
| March 2024 | 5 |
| April 2024 | 5 |
| May 2024 | 10 |
| June 2024 | 10 |
| July 2024 | 10 |
| August 2024 | 20 |
| September 2024 | 20 |
| October 2024 onwards | 30 |
If the pharmacy owner wishes to stop providing the service, they must notify NHS England that they are no longer going to provide the service via the MYS platform, giving at least 30 days’ notice prior to the cessation of the service. The pharmacy owner may be asked for their reason for withdrawal from the service.
Pharmacy owners must have a Standard Operating Procedure (SOP) for the service, which all staff participating in provision of the service must be familiar with and follow.
Various pharmacy support organisations provide template SOPs which their members can personalise for use in their pharmacy.
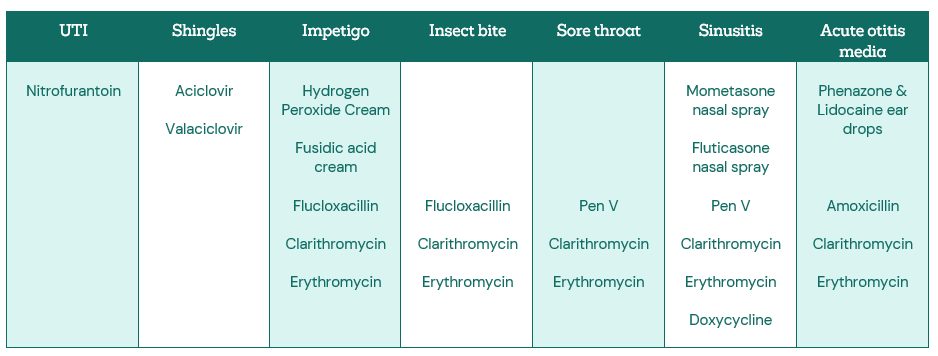
Pharmacy First Clinical pathways – medicines included in the PGDs and medicines protocol
Useful information
Promoting the service to the Public
Posters for display within pharmacy
- PF-Inside-the-Pharmacy-poster-1
- PF-Inside-the-Pharmacy-poster-2
- PF-Inside-the-Pharmacy-poster-3
- PF-Inside-the-Pharmacy-poster-4
- PF-Inside-the-Pharmacy-poster-5
- PF-Inside-the-Pharmacy-poster-6
- PF-Inside-the-Pharmacy-poster-7
- PF-Inside-the-Pharmacy-poster-8
Posts for more general use
- PF-Generic-poster-1
- PF-Generic-poster-2
- PF-Generic-poster-3
- PF-Generic-poster-4
- PF-Generic-poster-5
- PF-Generic-poster-6
- PF-Generic-poster-7
- PF-Generic-poster-8
Small flyers for prescription bags
Pharmacy First Inclusion Criteria
Why should you go to your pharmacy first?
FAQs:
Q. How should I dispose of otoscope and ear thermometer covers and tongue depressors following use in the examination of a patient?Within the Health Technical Memorandum 07-01: Safe and sustainable management of healthcare waste such single use items are classified as offensive waste – see page 81 of the document (2022 version). This is not clinical waste, but may contain body fluids, secretions or excretions and it needs to be disposed of in yellow and black-striped ‘tiger’ bags.



